A 70 year old male with Fever , dribbling of urine,dry cough,myalgia
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
A 70 year old male patient resident of chityal daily labour by occupation presented with chief complaints of fever since 15 days
Dribbling of urine since 10 days
Myalgia since 5 days
Dry cough since 2 days
History of presenting illness:
Patient was apparently aymptomatic 15 days back then he had high grade fever associated with chills ,which is intermittent for which he went to local hospital and took medicine for 7 days,no significant relief from symptoms ,so he went to hospital in Chotuppal and was diagnosed with Typhoid fever.came here for further management.
Dribbling of urine since 10 days associated with burning micturition at times not associated with dysuria ,haematuria.
History of myalgia since 5 days
History of dry cough since 2 days.
Past history:
Patient had complaints of severe low back pain, paresthesia in the lower limbs and sough for consultation and underwent L-S spine fixation 18 yrs back.
He was diagnosed with Diabetes Mellitus on regular health checkup which were conducted in the Health center; and started on Oral hypoglycemic agents since 12 yrs
History of loin pain radiating to the groin on the right side 5 yrs back; treated conservatively.
Personal History:
Non vegetarian.
Sleep was adequate.
Appetite decreased.
Bowel and bladder movements are regular
He used to smoke 12 beedis per day since he was 15 Yrs and stopped 18 yrs back.
He consumes alcohol occasionally since he was 15 Yrs.
No known allergies to drugs.
General examination:
Patient was conscious and coherent.
Pallor: Absent
Canosis , clubbing ,lymphadenopathy, bilateral pedaledema absent
Febrile, Temp : 102°F.
PR: 102 bpm; RR: 19 cpm; BP: 110/80mmHg; GRBS: 247 mg/dl.
CVS: S1, S2+; R/S: BAE+, Clear;
P/A: Soft, Non tender, BS+,;
CNS: HMF intact,; NFND.
INVESTIGATIONS:
Chest X Ray PA View:
X ray Abdomen and Pelvis:
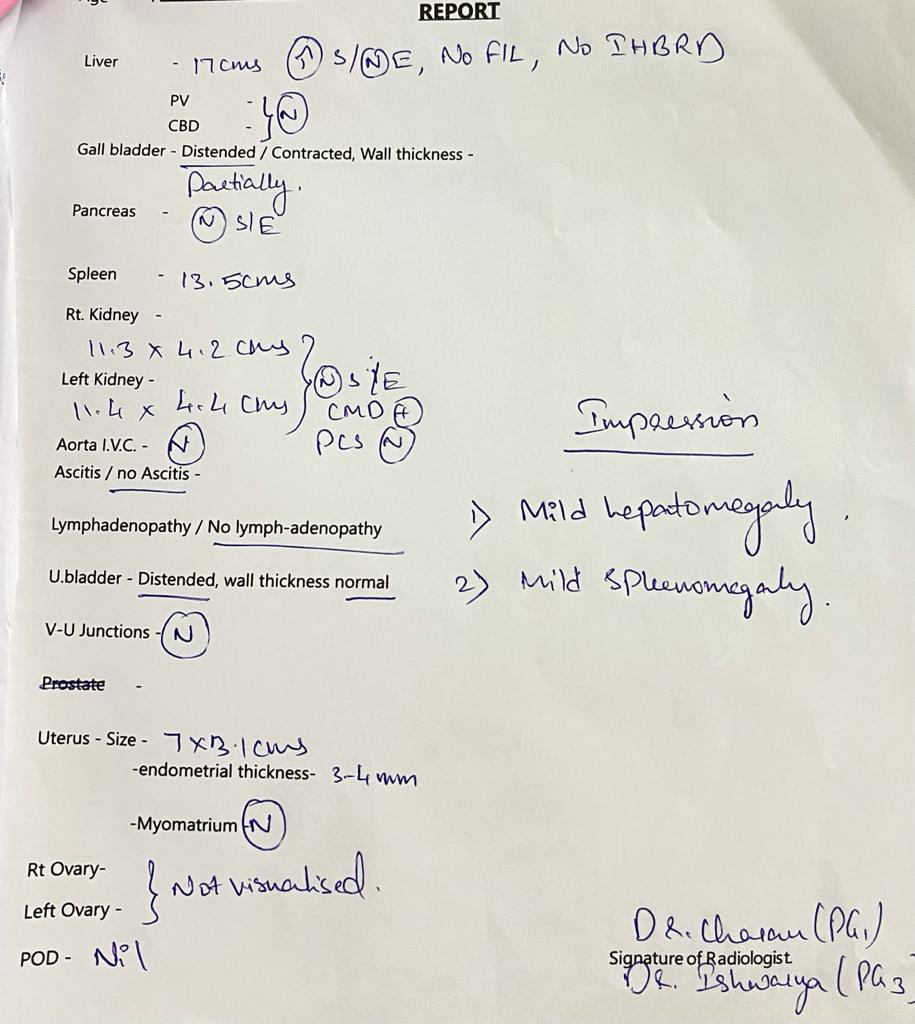
Ultrasound of Abdomen:
Colour Doppler 2D Echo:
PROVISIONAL DIAGNOSIS:
Pyrexia under evaluation
TREATMENT:
1. IVF NS/RL @75 ML/HOUR.
2. INJ. NEOMOL 100ML /IV/TID.
3. INJ. ZOFER 4MG/IV/ SOS.
4. SYP. ARYSTOZYME 15ML/PO/TID.
5. GRBS 7• PROFILE.
6. VITAL MONITORING 4TH HOURLY.
7. I/O CHARTING.