46 yr old male with Shortness of Breath, Abdominal distension, pedal Edema.
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
A 47 year old male resident of Keshavapuram, Shephard by occupation presented with
Chief complaints:
Shortness of Breath since 6 years
Cough since 4 years
Abdominal distension since 3years
Puffiness of face since 3 years
Pedal Edema since 3 years.
History of presenting illness:
Patient was apparently asyptomatic 6 yrs back then he developed Shortness of Breath which was insidious in onset , gradually progressed from Grade1 to Grade 2 not associated with dyspnoes on lying down.
He had cough since 4 years which is associated with yellow coloured sputum.
He noticed abdominal distension since 3 years
He noticed puffiness of face since 3 years..
He noticed pedal Edema ( below the knee) since 3 years .
He had Hard stools since 10 days not mixed with blood .
Past History:
No similar complaints in the past .
Not a Known case of Diabetes mellitus, Hypertension, Tuberculosis,Asthma,coronary artery Disease, Epilepsy.
Surgical History- Underwent Cataract surgery in 2021
Treatment History- Used locally prescribed antacid tablets.
Family History
No member of the family has similar complaints.
Personal History
Appetite is normal.
Diet: Mixed
Bowel& bladder: Bowel - Hardstools since 10 days
Bladder movements regular
Sleep: Adequate
Addictions: He consumes Alcohol since 30 years (200 ml/ day) stopped 3months back
He smokes cigarette & beedi since 30 years 12/ day .
No food& drug allergies
Daily routine
He wakes up at 5 am and goes to animal shed and comes home at 8am eats rice at 10 am ,goes to work in farm and comes home by 6 pm ,used to consume alcohol occasionally and takes dinner by 9pm and goes to bed by 10 pm.
General examination
Patient is conscious coherent cooperative moderately bulit and nourished.
Pallor absent
Bilateral pedal edema prese
Generalised lymphadenopathy - Absent
Vitals :
Pulse rate -82 bpm , regular in rate rhythm and normal volume , bilaterally present
Bp:110/90 mm of Hg
Temp :99
Respiratory rate:20/ min
JVP - slightly elevated
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
CNS : Higher Mental functions Intact
No focal neurological deficits.
Cranial nerves intact.
Provisional Diagnosis:
Investigations:
Ultrasound Abdomen
2D Echo
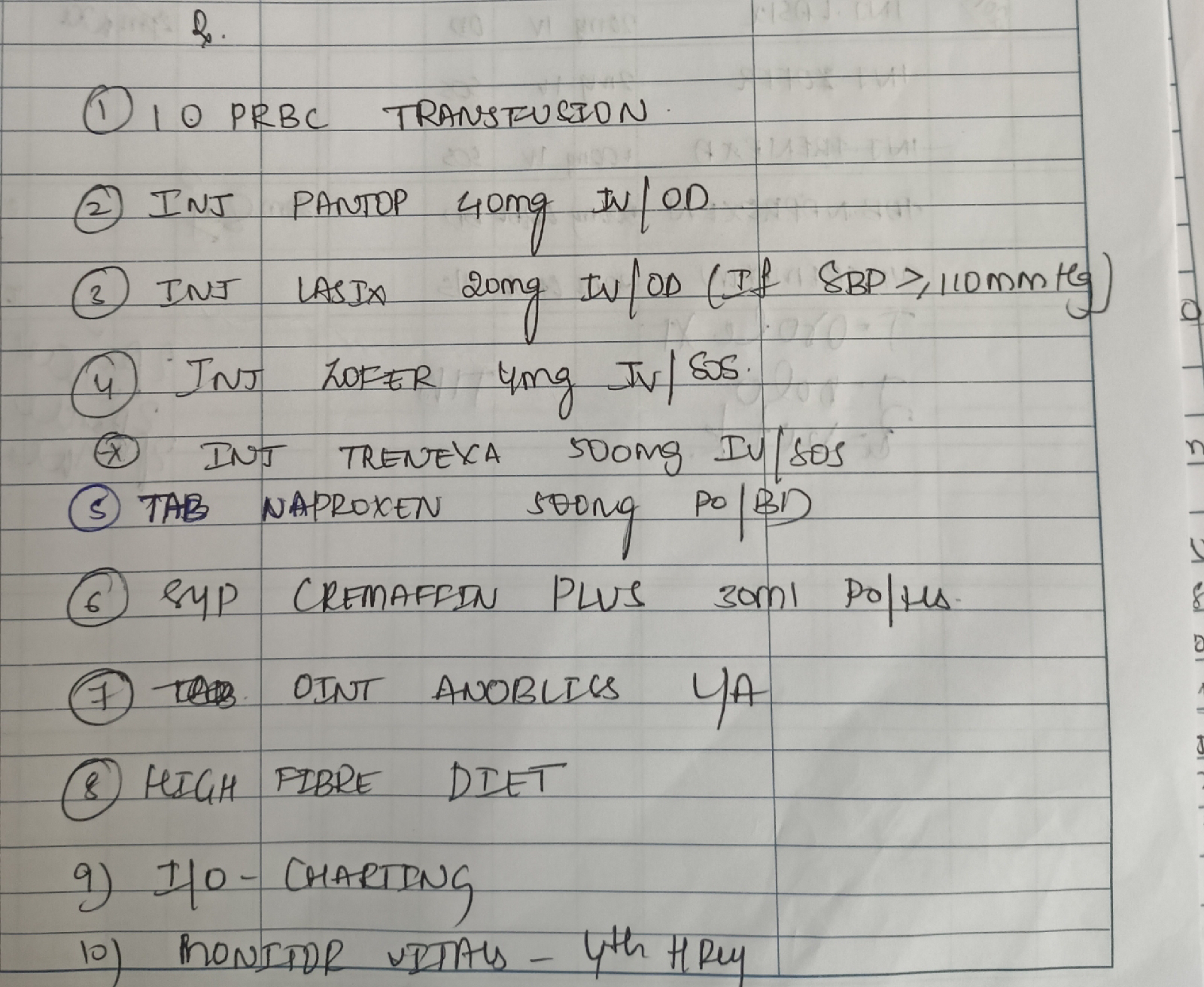
Treatment: